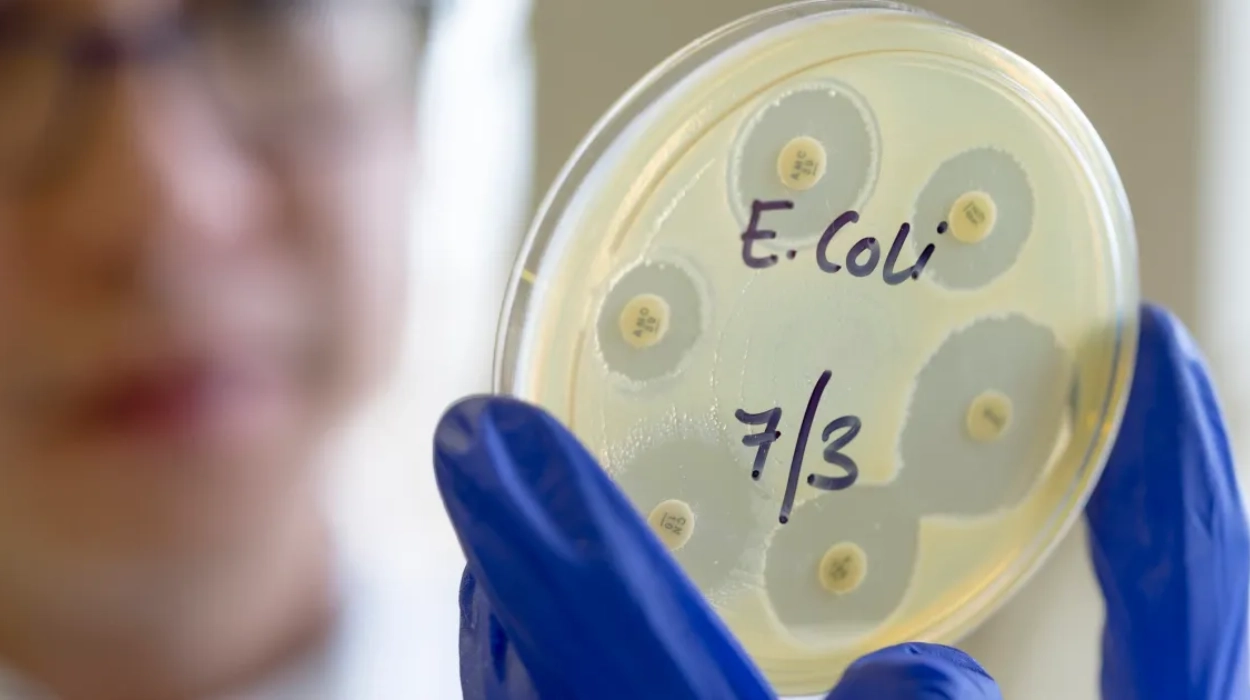
London (Parliament News) – An outbreak of over 100 E-coli cases prompts UK health warning. The UKHSA investigates potential food-related origins while cautioning against contact with contaminated environments. Public advised on hygiene practices.
The UK’s public health administration has sounded the warning over E-coli poisoning after an outbreak of more than 100 cases registered in less than two weeks. The UK Health Security Agency (UKHSA) stated that it is likely the outbreak is connected to “a nationally distributed food item or multiple food items.”
Are there any suspected sources of the outbreak?
It stated there is no evidence the outbreak is related to open farms, drinking water, or swimming in contaminated seawater, lakes or rivers. The health authority proved there have been 113 confirmed patients of Shiga toxin-producing E-coli (STEC), associated with the explosion, since 25 May. 81 cases are in IK, 18 in Wales, 13 in Scotland and one in Northern Ireland.
The cases range from children two to 79 years old. The bulk of cases are described as young adults.
Out of the 81 patients in England, 61 have given UKHSA statements related to food, travel and potential vulnerabilities, and of those 61 per cent were hospitalised. Typically, approximately 1,500 cases of this type of e-coli are seen in the UK in a year.
“Numbers of confirmed patients associated with this outbreak are anticipated to rise as further samples experience whole genome sequencing,” the UKHSA added. In December, it established that 30 cases of E-coli (STEC) had been registered across England and Scotland, where one person with the infection passed.
What precautions are recommended by health authorities?
In March, the university Boat Race’s organisers cautioned rowers not to enter the water on safety grounds after high levels of E-coli bacteria were uncovered in the River Thames along the course. Infections induced by STEC bacteria can lead to painful bloody diarrhoea, and sometimes more serious complications.
The UKHSA stated it is often transmitted by consuming contaminated food, but can also be spread through close connection with an infected person, as well as direct touch with an infected animal or its environment. The public has been urged to regularly wash their hands, follow food hygiene standards such as washing fruit and vegetables, and bypass visiting people in hospitals or care homes to avoid passing on the infection.
Darren Whitby, director of incidents and resilience at the Food Standards Agency, stated: “The FSA is working with UKHSA and relevant public health bodies to identify the source of the illness, which is likely to be linked to one or more food items.”